Zika Virus infection in pregnancy is a self-limited disease that generally lasts a few days up to two weeks. However, there may be a risk of microcephaly or abnormal neurologic development in the fetus. It is unknown at this time whether the timing of the infection in pregnancy or the severity of the symptoms in the pregnant person influence the risk to the fetus. Travellers are recommended to have early consultation with a health care provider regarding questions about Zika virus in pregnancy.
Nova Scotia recommendations for screening pregnant persons is oulined in the Zika Virus Testing Algorithm, and are summarized below.
Screening Criteria:
- All pregnant individuals with a potential exposure to Zika virus require assessment, regardless of whether they develop symptoms.
- Potential exposure is defined as personal travel to a Zika affected area any time after the date of the last known menstrual period or unprotected sexual contact with a male partner who has traveled to a Zika affected area in the last 6 months.
- Refer to the Public Health Agency of Canada for the most recent travel health notices for updates about Zika Virus destination specific advisories.
Screening and Referral Process:
- Asymptomatic individuals with a potential Zika Virus exposure:
- Referral to IWK Health Fetal Assessment and Treatment Center (FATC).
- Offer Zika virus serology, as described in the Zika Virus Testing Algorithm.
- The Zika Virus Clinical Information Data Sheet must be completed and sent with the specimens to the Department of Pathology and Laboratory Medicine, Central Zone.
- Symptomatic individuals with a potential Zika Virus exposure:
- Referral to IWK Health Fetal Assessment and Treatment Center (FATC) .
- Blood collection for both Zika virus RNA detection and serology, and urine specimens Zika virus RNA detection, as described in the Zika Virus Testing Algorithm.
- The Zika Virus Clinical Information Data must be completed and sent with the specimens to the Department of Pathology and Laboratory Medicine, Central Zone.
*The timing of Zika virus serology is important. For an asymptomatic pregnant person, serology should be completed NO SOONER than three weeks following the last exposure. At this time Zika serology for male partners is not being offered in Canada.
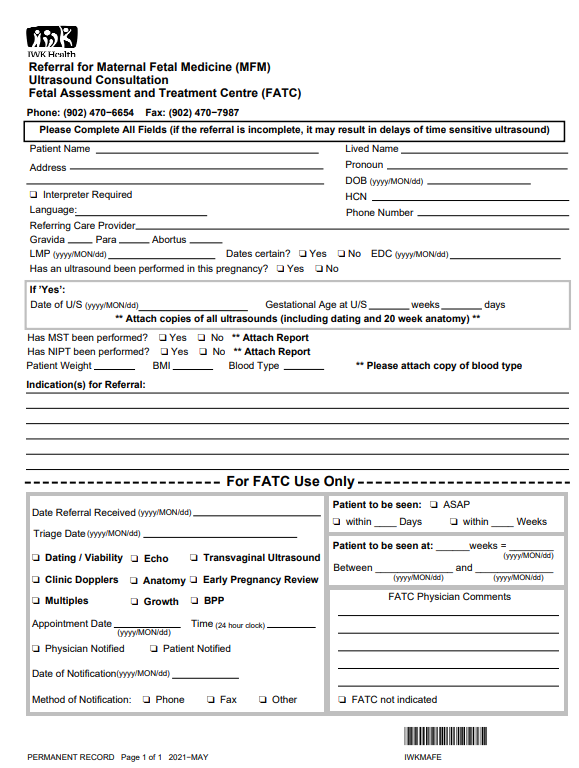
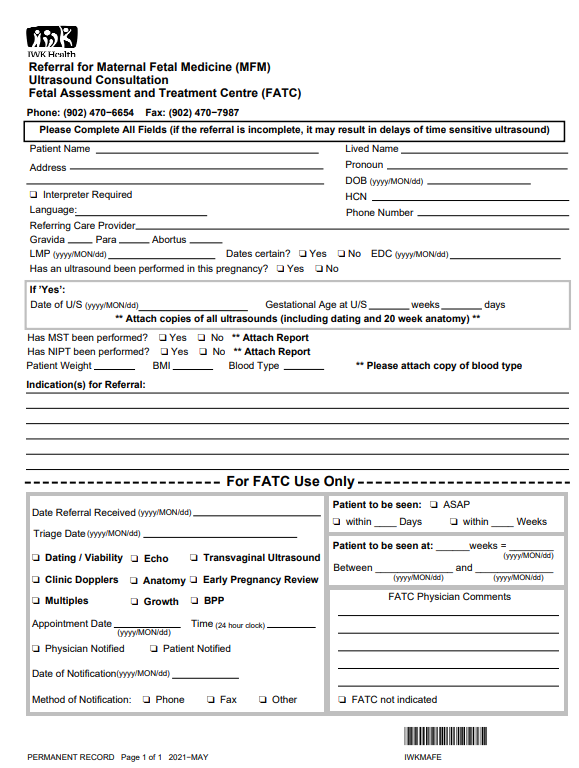
FATC Referral:
- Incude the following informaiton in the FATC referral:
- Date of the last know menstrual period (LMP) LMP.
- Circumstances of exposure in the context of gestational age (travel history or history of unprotected sexual contact with a male with potential exposure to Zika virus).
- The presence or absence of symptoms consistent with Zika virus in the pregnant person or their partner, including the timing of the appearance of symptoms, if any.
- Whether or not a blood sample has been sent for Zika serology and, if so, the date the sample was collected.
- The FATC referral form can be found HERE. A new form must be printed for each referral (due to the barcode) and the form must be faxed to FATC at 902-470-7987.
Prevention:
The risk of Zika virus is low in Canada but travelers to areas affected by current outbreaks should protect themselves from potential infection.
- Individuals should protect themselves frommosquito bites by using appropriate insect repellant, wearing protective clothing, and using mosquito nets.
- Public Health Agency of Canada recommends that those who are pregnant or considering becoming pregnant avoid travel to areas affected by current outbreak. Public Health Agency of Canada travel health notices.
- There is evidence that Zika virus can be transmitted sexually:
- Persons who may become pregnant should wait two months after returning from a Zika affected area before trying to conceive.
- Persons who are pregnant or may become pregnant should avoid sexual contact or use condoms with a partner who has recently travelled to a Zika affected area, and for at least six months after returning from the Zika affected area.
Additional Information:
|
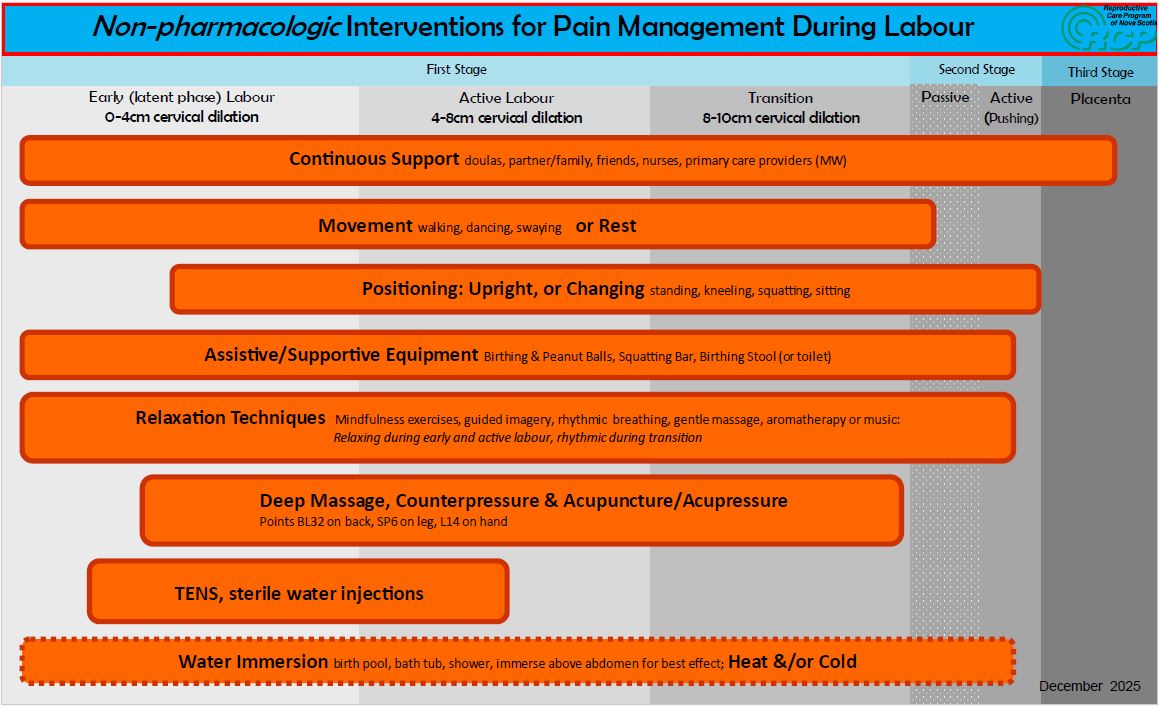
Labour is a dynamic process, with each birthing person experiencing the pain of labour differently. Effective pain management involves understanding the range of available strategies and choosing the options that best support comfort, control, confidence, and enhance coping throughout each stage of labour. This infographic outlines both non-pharmacologic and pharmacologic pain management techniques—highlighting practical, evidence-informed methods that can be used alone or in combination. By exploring these approaches, labouring individuals, care providers, and support persons can make informed decisions that align with personal preferences, clinical needs, and support the progression of labour.
|
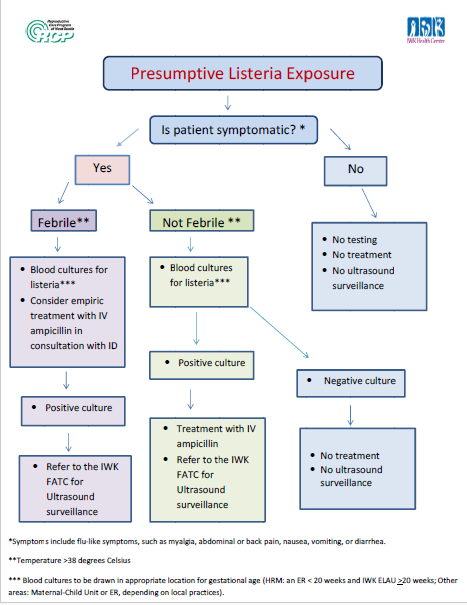
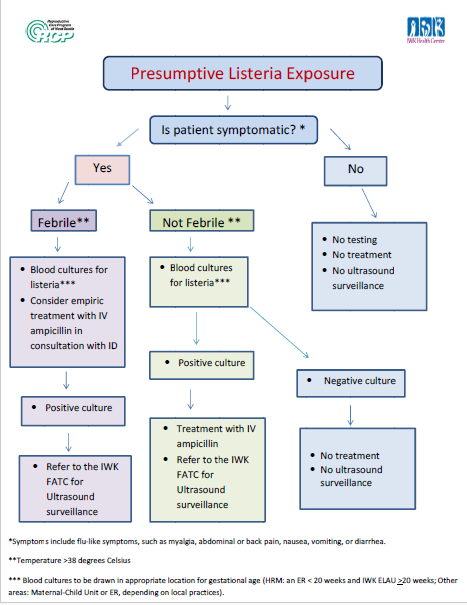
In response to recent questions about exposure to products that may have been contaminated with listeria, we would like to remind providers of a testing and treatment algorithm that was developed by the IWK and RCP for pregnant patient with presumptive listeria exposure.
Pregnant patients with a positive blood culture for listeria should be referred to the Fetal Assessment & Treatment Centre (FATC) for surveillance.
The FATC referral form can be found on the IWK website.
Note: A new form must be printed for each referral (due to the barcode) and the form must be faxed to FATC at 902- 470−7987.
|
This resource has been developed by care providers at IWK Health with contribution from the Reproductive Care Program. The goal is to offer prenatal care providers across Nova Scotia with an information resource that will guide pregnant persons regarding fetal movement.
Feel free to print the resource for easy reference and / or posting within your clinical spaces.
|
This practice resource provides prenatal care providers with screening and treatment guidance for anemia in pregnancy, based on evidence as of the date of the most recent version. The algorithm distinguishes between the types of anemia that may be encountered, presents the health professional with the most appropriate treatment options, and provides recommendations for follow-up assessments.
|
This practice resource, developed in September 2021 and revised in February 2022, provides information to care providers related to a new approach to GDM screening in Nova Scotia. The practice resource has been informed by evidence and has been adapted specifically to Nova Scotia’s context and population of pregnant persons. It includes the Diabetes Care Program of Nova Scotia GDM screening practice algorithm and information related to the interpretation of testing results.
In January 2022, Central Zone Pathology and Laboratory Medicine issued a memo outlining the process for ordering HbA1C based on the new provincial approach to GDM screening.
In June 2022, the Diabetes Team at the IWK issued a memo outlining operational changes in their approach to diabetes and ultrasound surveillance for diabetic patients.
Additionally, you may watch New Approach to GDM Screening in Nova Scotia, a recorded presentation given by Dr. Jillian Coolen on October 25, 2021 as part of RCP's Webinar Series.
Pregnancy and Diabetes: Approaches to Practice (2021): This resource, published by the Diabetes Care Program of Nova Scotia (DCPNS), provides health care providers with additional information in support of recognized Clinical Practice Guidelines for the management of pregnancy complicated by diabetes.
|
The Nova Scotia Vaccine Expert Panel has updated resources for care providers to use with pregnant and breastfeeding individuals to guide discussion about COVID-19 vaccination. This information is specific to adult immunization.
In addition to these documents, the IWK has produced a video to help individuals make an informed choice about whether to get the COVID vaccine while they are pregnant, trying to get pregnant or breastfeeding. The video is hosted on the IWK public website: https://www.iwk.nshealth.ca/COVID-19/vaccine-info-for-pregnant-or-breastfeeding

For more resources related to the care of pregnant patients and their newborns affected by COVID-19, please refer to our COVID-19 Resources page.
|
Accurate assessment of gestational age is crucial:
- to determine viability of extreme preterm birth
- to properly interpret maternal serum screening for aneuploidy
- to prevent post term induction of labour and
- to optimize obstetric care including avoiding inappropriate perinatal interventions.
Consistent approaches to gestational age assessment must also be taken to optimize accuracy.
This provincial guideline has been revised to reflect the recommendations of national professional organizations and local experts, within the context of Nova Scotia perinatal care provision. As such, these guidelines may differ from those found in other jurisdictions. The RCP acknowledges the Divisions of Maternal Fetal Medicine (MFM) and Neonatal Perinatal Medicine (NPM) at the IWK Health Centre, for their collaboration in producing this guideline.
|
Syphilis and Screening in NS for Pregnant Persons and Newborns
The rate of syphilis in Canada has been steadily rising in recent years, becoming a significant public health concern. A surge in syphilis infection among women of childbearing age has led to more cases of congenital syphilis (transmission from the pregnant person to the fetus during pregnancy), which can result in severe health outcomes or death in newborns. An infographic created by the Public Health Agency of Canada provides a visual aid depicting the increase in syphilis rates in Canada. Cases of syphilis in pregnancy and confirmed cases of syphilitic stillbirth are reportable to Public Health. The rise in cases has led to national research exploring strategies to address infectious and congenital syphilis in Canada.

Screening
Screening recommendations for syphilis during the antenatal and postpartum periods, and for newborns are provided below. These recommendations have been in place since 2020, were adapted from national guidelines, and remain in place until further notice. See the letter to care providers from January 2020 for additional practice guidance regarding consultation, testing and treatment.
Perform syphilis serology:
- Early in pregnancy for all pregnant persons.
- Repeat for all pregnant persons at 24 -28 weeks gestation.
- For patients considered at high risk for syphilis, repeat syphilis serology at the time of birth.
- For patients considered at high risk for syphilis, repeat syphilis serology at the time of birth.
- In pregnant persons who experience a stillbirth from 20 weeks gestation onward.
- In pregnant persons who have NOT had the recommended syphilis serology during pregnancy, complete the screening prior to discharge following birth.
- In infants presenting with symptoms or signs compatible with early congenital syphilis even if the parent was seronegative at birth, due to the possibility of a very recent parental infection.
Nova Scotia Department of Health and Wellness Syphilis Surveillance Guidelines
The Nova Scotia Department of Health and Wellness have updated the Syphilis Surveillance Guidelines and they are now available. The update comprises the addition of new stages for congenital syphilis, including late congenital syphilis and syphilitic stillbirth. Surveillance Guidelines for congenital syphilis and non-congenital syphilis have been separated into two documents, both of which also contain guidelines for identifying syphilis outbreaks. For more information please access the Syphilis section of the Communicable Disease Manual that is accessible on the Nova Scotia Department of Health and Wellness website.
Provincial Syphilis Outbreak: Recommendations for pregnant persons and newborns
As of January 20, 2020, the Office of the Chief Medical Officer of Health for Nova Scotia has declared a provincial syphilis outbreak. Across Canada syphilis outbreaks have been declared in most provinces/territories, due to increasing rates of infection. Changes to recommendations for pregnant women and newborns are outlined in the documents below:
|
The Canadian Paediatric Society (CPS) has recommended moving from universal newborn ocular prophylaxis, to universal prenatal screening for Neisseriae gonorrhoeae (GC) and Chlamydia trachomatis (CT) and treatment of those with positive results in order to eradicate infection and prevent intrapartum transmission to the newborn.
As universal ocular prophylaxis is eliminated from routine newborn care, functions of the health system must be optimized and synchronized to prevent ON. RCP has partnered with clinical experts and stakeholders from across NS to produce these resources, which are designed to offer guidance for the prevention of ON:
|
Key messages for health care providers
- Black-legged or deer ticks (BLT) are found throughout Nova Scotia. Preventing a BLT bite is the most effective way to prevent Lyme disease. Risk reduction strategies include using DEET-containing insect repellant (safe to use in pregnancy) and careful ‘tick checks’ after being in grassy or wooded areas, including a park or yard. Immediate and correct removal of an attached BLT is key to prevention. For advice about tick removal see: https://novascotia.ca/dhw/CDPC/lyme.asp.
- Prophylaxis may be considered. A single 200 mg dose of doxycycline, which is not contraindicated for pregnant women, may be offered if all of the following criteria are met.
- BLT attached for > 24 hours, AND
- antibiotic prophylaxis is given < 72 hours from tick removal, AND
- the bite occurred in an area considered at higher or moderate risk for Lyme disease, which is most of NS. For risk level by NS County see map at this link: https://novascotia.ca/dhw/CDPC/lyme.asp.
- The risk of Lyme disease after a bite from an infected BLT is low (1.2%-3.2%). However, if a bite occurs advise observation for signs and symptoms for 30 days, even if there has been prophylaxis.
- Think about Lyme disease in your differential for a patient presenting with new onset febrile illness, especially when associated with a localized skin lesion. Early infection is a clinical diagnosis. The sensitivity of two-tiered serologic testing, the recommended testing standard in Canada and the US, is < 50% in early, localized Lyme disease. The test performs well in early disseminated and in late Lyme disease. For information about testing see: https://novascotia.ca/dhw/cdpc/documents/statement_for_managing_LD.pdf.
- Treatment for pregnant women with Lyme disease is similar to treatment for the general adult population, with the exception that treatment doses of doxycycline are contraindicated in pregnancy. With 10-28 days of oral antibiotic treatment, 95% of cases of Lyme disease are resolved. For treatment recommendations see: https://novascotia.ca/dhw/cdpc/documents/statement_for_managing_LD.pdf
- There is not enough evidence to confirm that Lyme disease during pregnancy has adverse effects for the fetus. In addition, no adverse effects for the fetus have been observed when the pregnant woman receives appropriate antibiotic treatment for her Lyme disease.
For more information about Lyme disease, refer to the following resources:
From the Government of Canada and the Public Health Agency of Canada
From the Nova Scotia Department of Health & Wellness
|
A detailed guide and reference for prenatal care providers using the Nova Scotia Prenatal Record to document assessment, investigation and treatment during pregnancy. Includes instructions on assembly of the prenatal record, a glossary of terms related to pregnancy and prenatal care, details on completing each section of the record, guidelines for antenatal screening and related resources.
|
The Nova Scotia guidelines for antenatal laboratory screening and testing were revised and re-released in 2024. The guidelines are available in a convenient printable card format. The companion document to the new Nova Scotia Prenatal Record provides detailed information on applying these guidelines.
|