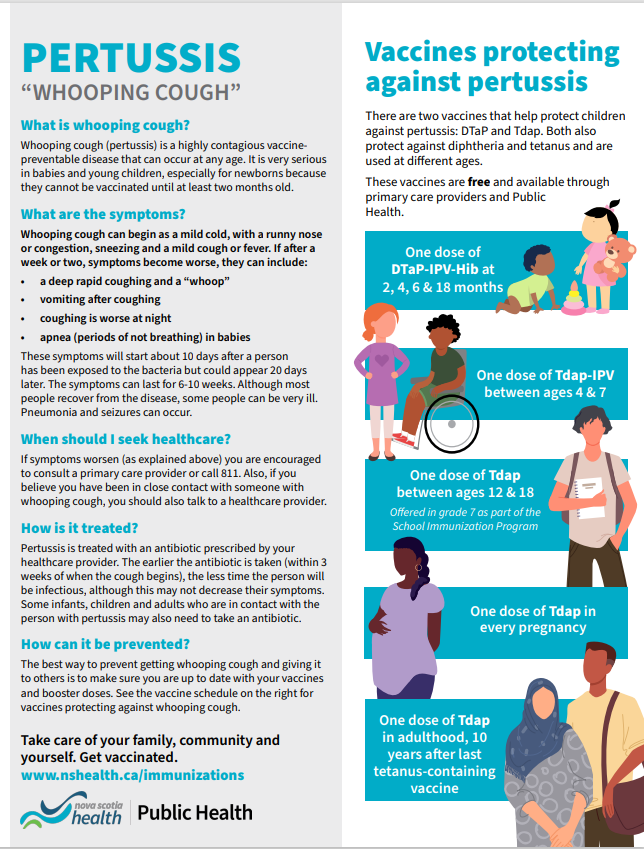
Provincial Pertussis Information from Public Health
Canada is seeing an overall increase in pertussis (whooping cough) cases, including here in Nova Scotia. Pertussis is a vaccine preventable disease that can be easily spread from person to person. It is spread by close contact with drops of fluid from the nose and throat of someone who has the disease.
Pertussis is very serious for babies and young children, especially newborns because they cannot be vaccinated until at least two months of age and can become extremely sick from pertussis. For this reason pregnant persons are strongly encouraged to get a dose of the pertussis vaccine (Tdap) during the third trimester of pregnancy, as the immunization offers some protection for newborns.
NS Public Health is requesting that care providers and community partners share information about pertussis prevention, signs and symptoms with pregnant persons and those with new babies, so they will be better informed about options for protecting their children. Please share the letter and infographic with the people you serve and post the infographic in public spaces.
As a reminder for healthcare providers, anyone suspected to have pertussis should have a nasopharyngeal (NP) swab to rule in or out the diagnosis. These swabs should preferably be done prior to starting antibiotics. Pertussis is a notifiable disease and all confirmed diagnoses must be reported to Public Health. This document provides details on how to report notifiable diseases. More information about pertussis is also available at www.nshealth.ca/pertussis .
National Advisory Committee on Immunization(2018)
In February of 2018, the National Advisory Committee on Immunization issued updated guidelines for pertussis vaccination in pregnancy.
https://www.canada.ca/en/public-health/services/publications/healthy-liv...
Tdap in Pregnancy:
- Immunization with Tdap vaccine should be offered in every pregnancy at 27-32 weeks of gestation, regardless of previous Tdap immunization history.
- Tdap immunization in pregnancy has been shown to protect infants against pertussis in the first three months of life. The safety of the Tdap vaccine during pregnancy is well established.
- Based on safety and effectiveness data, the ideal timing for immunization is 27-32 weeks of gestation. Immunization between 22-26 weeks may be considered for specific clinical or operational reasons, e.g. increased risk of preterm delivery. Although NACI supports immunization between 13-26 weeks, 22-26 weeks covers most preterm babies.
- Immunization until the end of pregnancy should be considered as it has the potential to provide partial protection (four weeks are required for optimal transfer of antibodies and direct protection of the infant against pertussis). In addition, there may be indirect protection through breast milk.
- Women who were not immunized during pregnancy should receive Tdap as soon as possible after birth to protect the baby from coming into contact with pertussis. Immunization is particularly important if the baby is preterm.
- If Tdap immunization was provided early in pregnancy (e.g. prior to recognition of pregnancy), it is not necessary to re-immunize after 13 weeks of gestation.
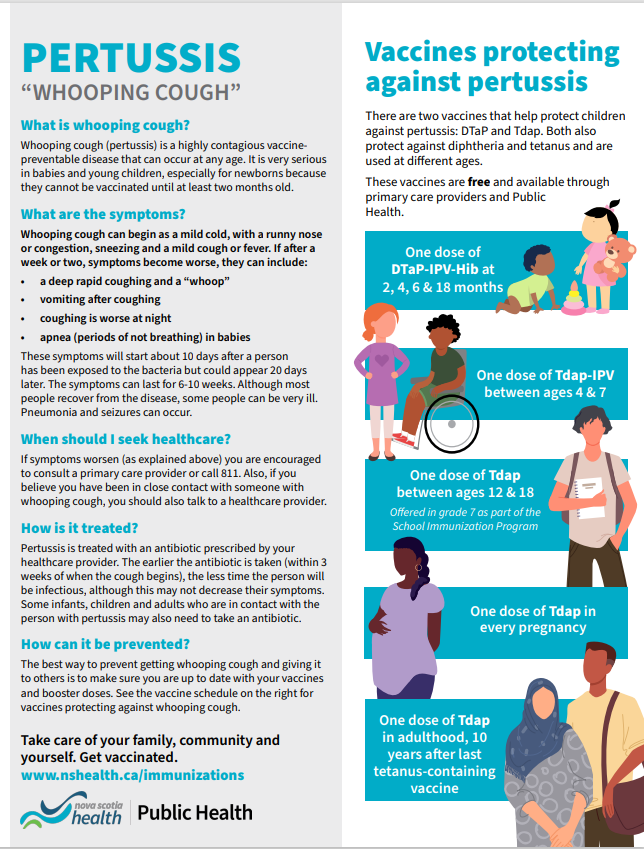
In addition, all caregivers and close contacts, both children and adults, should be up to date with their pertussis immunization. The Nova Scotia Routine Immunization schedule is available here:
https://novascotia.ca/dhw/cdpc/documents/Routine-Immunization-Schedules-...
Infants and young children are at particular risk of contracting pertussis until they have completed their primary immunization series. For maximum protection, children need a primary series of pertussis-containing vaccine at two, four, and six months followed by booster doses at 18 months, between four to six years of age, and again as part of the school-based immunization program, which in Nova Scotia, occurs in Grade 7.
The best way to prevent mortality and significant morbidity from pertussis is for health care providers to:
- offer one dose of pertussis containing vaccine (Tdap) to all pregnant women, ideally at 27-32 weeks of gestation. An earlier gestation may be chosen in some circumstances;
- ensure that infants and young children are immunized according to the recommended schedule; and
- recommend that caregivers and close contacts of infants and young children receive a pertussis immunization.